Multiple Sclerosis Explained: From Early Signs to Modern Therapies
Multiple sclerosis (MS) is a chronic, immune-mediated disease of the central nervous system (CNS), which includes the brain, spinal cord, and optic nerves. It is characterized by inflammation, demyelination, and neurodegeneration. The damage occurs when the immune system attacks the protective myelin sheath around nerve fibers, leading to scarring (sclerosis) and disrupted nerve signaling. Over time, this can result in cumulative disability.
Multiple sclerosis (MS) is a chronic, immune-mediated disease of the central nervous system (CNS), which includes the brain, spinal cord, and optic nerves. It is characterized by inflammation, demyelination, and neurodegeneration. The damage occurs when the immune system attacks the protective myelin sheath around nerve fibers, leading to scarring (sclerosis) and disrupted nerve signaling. Over time, this can result in cumulative disability.
MS most commonly affects young adults between the ages of 20 and 40, with women affected nearly three times more often than men. While no cure currently exists, early diagnosis and advances in treatment have significantly improved outcomes.
Pathogenesis
The development of MS is complex and involves genetic, environmental, and immunological factors.
Genetic susceptibility
The strongest genetic association is with HLA-DRB1*15:01, a human leukocyte antigen allele.
Having a first-degree relative with MS increases risk, though inheritance is not direct.
Environmental and lifestyle triggers
Vitamin D deficiency and low sunlight exposure.
Viral infections: Strong evidence links Epstein-Barr virus (EBV) infection to increased MS risk.
Smoking: Raises both the risk of developing MS and disease severity.
Obesity in adolescence: Emerging as a significant risk factor.
Immune system dysfunction
T cells and B cells become autoreactive and attack myelin.
Inflammatory cytokines (e.g., IFN-γ, TNF-α, IL-17) disrupt the blood-brain barrier, allowing immune cells to infiltrate the CNS.
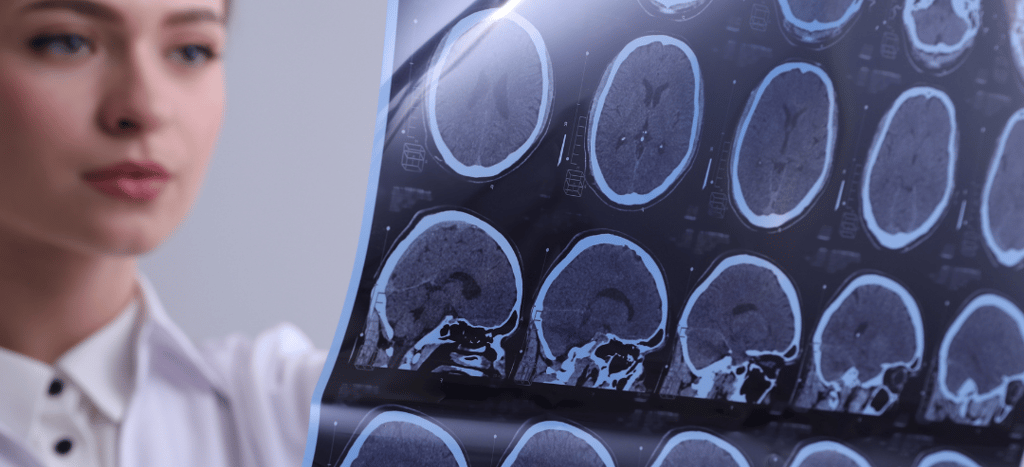
This results in plaques (lesions) of demyelination and axonal loss, seen on MRI scans.
Symptoms of MS
MS is often called “the disease of a thousand faces” because symptoms vary widely depending on which part of the CNS is affected.
Visual symptoms
Optic neuritis: blurred or lost vision, eye pain, color vision changes.
Motor symptoms
Muscle weakness, spasticity, poor coordination, tremors.
Sensory symptoms
Numbness, tingling, burning sensations.
Balance and mobility issues
Unsteady gait, dizziness, problems with coordination.
Cognitive and emotional changes
Memory difficulties, slowed processing, depression, anxiety.
Other systemic symptoms
Severe fatigue (one of the most disabling features).
Bladder and bowel dysfunction.
Sexual dysfunction.
Types of MS
The course of MS can differ significantly among patients.
Relapsing-Remitting MS (RRMS)
About 85% of patients at onset.
Defined by episodes of new or worsening symptoms (relapses) followed by partial or complete recovery (remission).
Secondary Progressive MS (SPMS)
Initially RRMS, later transitions to a phase of gradual, steady worsening with fewer relapses.
Primary Progressive MS (PPMS)
About 10–15% of cases.
Characterized by steady decline from the beginning, without relapses or remissions.
Progressive-Relapsing MS (PRMS)
Rare; progressive from onset but with superimposed relapses.
Diagnosis
Diagnosing MS is challenging because no single test confirms the disease. A combination of clinical, radiological, and laboratory evidence is required.
Clinical evaluation
Neurological examination to assess reflexes, coordination, vision, strength, and sensation.
MRI imaging
Gold standard for detecting lesions in the brain and spinal cord.
Contrast-enhanced MRI can show active inflammation.
Cerebrospinal fluid (CSF) analysis
Lumbar puncture often reveals oligoclonal bands, indicating immune activity in the CNS.
Evoked potentials
Measure slowed electrical conduction in optic nerves or spinal pathways.
Diagnostic criteria
The 2017 revised McDonald criteria allow earlier diagnosis by combining clinical attacks, MRI evidence, and CSF findings.
Treatment
While there is no cure, treatment focuses on slowing progression, reducing relapses, and managing symptoms.
Disease-Modifying Therapies (DMTs)
These medications target the immune system to reduce relapses and new lesion formation.
Injectable therapies: Interferon beta, glatiramer acetate.
Oral therapies: Fingolimod, dimethyl fumarate, teriflunomide, siponimod.
Infusion therapies:
Natalizumab (monoclonal antibody against α4-integrin).
Ocrelizumab (anti-CD20, effective for both RRMS and PPMS).
Alemtuzumab (anti-CD52, potent but with higher safety concerns).
Managing Acute Relapses
High-dose corticosteroids (e.g., methylprednisolone) reduce inflammation.
Plasma exchange may be considered for severe relapses not responding to steroids.
Symptom Management
Spasticity: Baclofen, tizanidine, physiotherapy.
Fatigue: Amantadine, modafinil, energy conservation strategies.
Bladder dysfunction: Anticholinergic drugs, pelvic floor therapy.
Depression/anxiety: Counseling and antidepressants.
Rehabilitation and Lifestyle
Physical therapy, occupational therapy, speech therapy.
Regular aerobic and strength exercise to preserve mobility.
Vitamin D supplementation.
Stress reduction, mindfulness, and balanced nutrition.
Prognosis and Outlook
MS is a highly variable disease. Some people experience mild symptoms for decades, while others may develop significant disability. Advances in DMTs have transformed MS from a disease often associated with early disability to one that can be managed long-term with improved quality of life. Early and consistent treatment, combined with rehabilitation, plays a key role in maintaining independence.
References:
Goldenberg MM. Multiple sclerosis review. P T. 2012;37(3):175–184.
Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–173. doi:10.1016/S1474-4422(17)30470-2.
Hauser SL, Cree BAC. Treatment of multiple sclerosis: a review. Am J Med. 2020;133(12):1380–1390.e2. doi:10.1016/j.amjmed.2020.05.049.
Montalban X, Gold R, Thompson AJ, et al. ECTRIMS/EAN guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler. 2018;24(2):96–120. doi:10.1177/1352458517751049.
Clinical Resources for Patients
National Multiple Sclerosis Society (U.S.): www.nationalmssociety.org
Multiple Sclerosis International Federation (MSIF): www.msif.org
MS Trust (UK): www.mstrust.org.uk
Mayo Clinic MS Resource Center: mayoclinic.org
